Understanding Cough in Children
Cough is one of the most common reasons parents bring their children to see the paediatrician. It can feel worrying and overwhelming, especially when you’re unsure what’s causing it, how serious it is or when your child needs medical attention. This guide explains why children cough, what you can do at home, and when to seek help.
What Is a Cough and Why Does It Happen?
A cough is an important protective reflex that facilitates the clearance of microbes, allergens, foreign particles and accumulated secretions from the airways through signals transmitted to the brain from the receptors found in both the upper and lower respiratory tract and elsewhere.
Because cough is protective and gives us valuable information about what may be happening, we usually focus on treating the cause, rather than suppressing the cough itself.
Common Causes of Cough in Children
Viral Infections
Viral infections are the most frequent reason children cough, especially those who attend nursery, playgroups, or school. This can sometimes make it feel like your child is “always unwell.”
Viruses can affect the upper airways (like colds or laryngitis) or the lower airways (such as bronchiolitis or viral-induced wheeze).
Typical viral coughs may:
- Start as a dry tickly or irritative cough
- Become wetter as mucus develops
- Peak in the first few days and usually settle within 1–2 weeks
Bacterial Infections
These are less common but tend to cause more severe illness. Children may experience:
- Progressive worsening fevers
- Pain and swelling
- Purulent discharge
- Breathing difficulty or chest pain if the lower respiratory tract is affected (e.g. bronchitis or pneumonia)
These infections generally need medical assessment.
Allergies
Allergies to tiny particles like pollen, dust mites, or pets may cause:
- Runny or blocked nose
- Itchy, watery eyes, puffy eyelids
- Sneezing
- Cough
Symptoms may come and go with exposure but could become more persistent and disruptive if not recognised early.
Asthma
Asthma is more commonly diagnosed in children over 5 years old.
Triggers include allergens, exercise, infections, weather changes, or irritants.
Children may experience:
- Coughing, especially at night
- A wheezing or whistling sound when breathing, especially when exhaling
- Chest tightness
- Recurrent episodes of breathing difficulty
Gastroesophageal Reflux
In babies, reflux of stomach contents into the upper airway can cause coughing.
Choking
Young children often explore the world by putting objects in their mouths. Food, toys, or small objects can become lodged in the airway and cause a sudden cough or breathing difficulty. Seek urgent medical help if choking is suspected.
Other Possible Triggers
- Exposure to cigarette or e-cigarette smoke
- Dust or chemical substance inhalation
- Food allergens
What Parents Can Do at Home
Babies Under 1 Year
Focus on comfort and gentle care:
- Saline nasal drops or spray before feeds and naps to make sure you baby keeps feeding and rests as well as possible
- Gentle suctioning of visible mucus
- Slight mattress elevation (about 30°)
- Humidifier or saline nebuliser could help soften the deeper mucus and ease coughing and breathing
Any cough in babies under 3 months should be reviewed promptly by a paediatrician.
Children 1–6 Years
If possible, help your child describe where their cough is coming from.
For a tickly dry throat cough:
- A small amount of honey (½ tablespoon) may help soothe irritation (do NOT give honey to children under 1 year)
- Over-the-counter throat sprays may provide temporary relief
For a wet / productive cough:
Help your child clear the mucus by using saline nasal sprays, a humidifier, or a saline nebuliser. Use these treatments mainly for comfort — for example, at times when the cough is most bothersome — rather than constantly through the day.
In general, over-the-counter cough medicines are not recommended in young children as they have limited efficacy and may carry safety risks, including toxicity or accidental overdose.
Children Over 6 Years
Parents may help by:
- Using honey, lozenges or throat sprays to relieve throat irritation
- Supporting mucus clearance as described above
- Considering over-the-counter antihistamines if the cough appears to follow exposure to an allergen (seek medical advice if unsure)
How Parents Can Monitor a Child’s Cough
The checklist below can help you keep track of your child’s symptoms, understand how the illness is progressing, and prepare helpful information if you need to visit a paediatrician:
- When did the cough start?
- Do you know what may have triggered it? (for example: a fever, allergy exposure, exercise, or certain foods)
- What does the cough sound like? If it seems unusual, a short video recorded at home can be very useful, as children may not cough during the consultation.
- When is it worse—day or night? Does it affect your child’s activity level, appetite, behaviour, or sleep?
- Is the cough getting better or worse over time?
- Have you tried any treatments? Please mention what you used and whether it helped.
- Are there any other symptoms besides the cough?
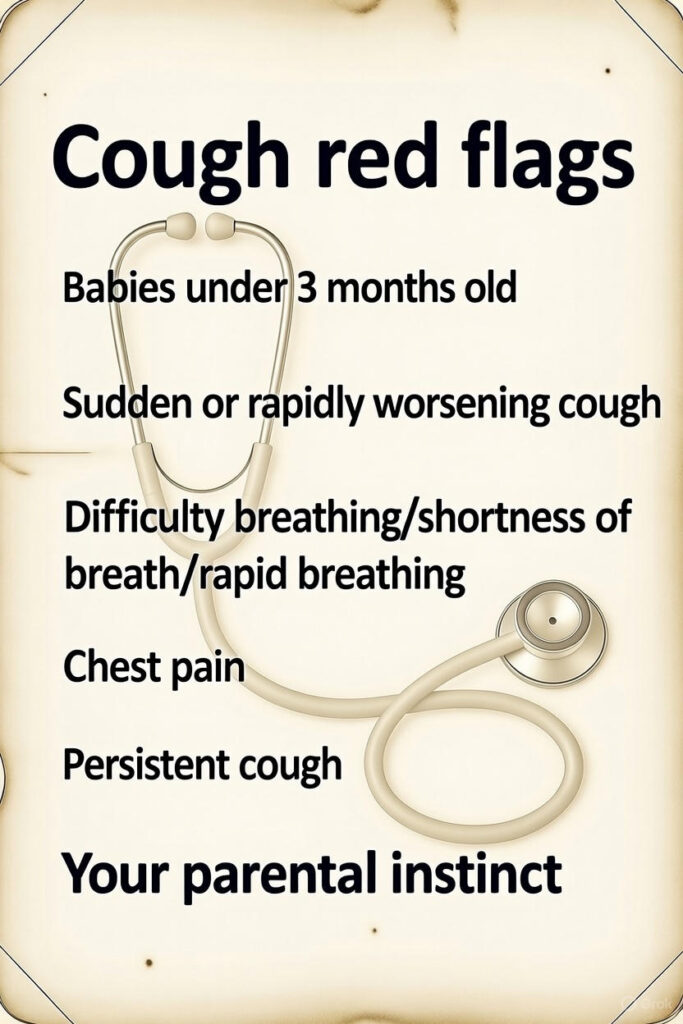
- Are there any warning signs (red flags)?
When to Seek Medical Help
Please seek urgent medical attention for your child if any of the following happen:
- Your child is under 3 months of age
- The cough starts suddenly or gets worse very quickly
- Your child has difficulty breathing, is breathing very fast, or you notice the skin pulling in around the ribs or neck
- Your child has chest pain
- The cough lasts longer than 3–4 weeks or is not improving as expected
- You are worried at any time — trust your instincts and seek medical advice
If you feel your child may need urgent treatment, please attend an urgent care facility or emergency department that is equipped to manage acute or severe illness, rather than a routine paediatric doctor’s office.
Final Takeaway
Cough is a protective reflex, not the enemy.
It helps clear the airways and signals what is happening inside the respiratory system.
In children, our goal is to treat the cause, not silence the cough.
If you are ever unsure, worried, or your child appears significantly unwell, always seek medical advice.
Disclaimer:
Dear parents,
The information shared on this blog is meant to support you by offering general guidance, education, and helpful tips from a paediatric perspective. However, every child is wonderfully unique, and the content here is not a substitute for personal medical advice.
Please remember that this blog doesn’t provide individual diagnoses, treatment plans, or medical care. If you have concerns about your child’s health, growth, behaviour, or well-being, it’s always best to reach out directly to your paediatrician or healthcare provider, who can give advice tailored specifically to your child.
While I do my best to ensure that everything shared here is accurate and up-to-date, medical knowledge changes so please use this blog as a helpful resource, not a medical authority.
Thanks for being here — It is my privilege to support you on your parenting journey!
Dr Manea

